HKU discovers a novel cellular therapy for bone marrow transplantation related complications
New hope for patients receiving bone marrow transplantation
30 Apr 2013
The University of Hong Kong discovers a novel cellular therapy for bone marrow transplantation (BMT) related complications, such as graft-versus-host disease (GVHD). Researchers successfully induce “antigen-specific CD8+ regulatory T cells” (Tregs), a special cell from human body, and then inject it to a “humanized mice” model equipped with complete human immune system for testing. They discover that the cell can effectively inhibit BMT-related GVHD while preserving general immunity of the host and the graft versus tumor effects, which brings hopes to the treatment of transplantation rejection. The study has been published earlier in a prestigious science journal Science Translational Medicine.
One of the researchers, Professor Lau Yu-lung, Doris Zimmern Professor in Community Child Health, Chair Professor of Department of Paediatrics and Adolescent Medicine, HKU Li Ka Shing Faculty of Medicine, indicates that, “Allogeneic BMT (i. e. the bone marrow is not from the patients themselves) might trigger severe rejection. Patients have to receive long-term radioactive and immunosuppression therapy before and after BMT. It might seriously affect the treatment outcome and the patients’ quality of life. This research discovers that ‘antigen-specific CD8+ regulatory T cells’, which is able to recognize BMT recipient’s antigen, can effectively suppress the immunoreaction specific to the recipient. This finding sheds light on the treatment of BMT rejection. ”
Research methods and findings
Regulatory T cell is a special kind of cell in human body which can effectively regulate the function of immune system and suppress overactive immune response. But this kind of cell is rare, only accounts for 1% of human peripheral blood cells. After spending 3 years on research, the team from Department of Paediatrics and Adolescent Medicine, HKU Li Ka Shing Faculty of Medicine, successfully developed an ex vivo system which can induce huge amount of “antigen-specific CD8+ regulatory T cells” in a short time.
The researchers only need small amount of peripheral blood from the donor and the recipient to conduct cell culture in the laboratory. They can then get enough “antigen-specific CD8+ regulatory T cells” for clinical use. They inject these cells to the humanized mice which received BMT for pre-clinical trial and observation afterwards. The result proves that, a single dose of “antigen-specific CD8+ regulatory T cells” can effectively inhibit the allogeneic GVHD. The survival rate and health condition of the mice significantly improve, while the general immune function of them remains normal.
The humanized mice used in this research contain a complete human immune system, which greatly mimic the allogeneic GVHD on human body. It can narrow the gap between animal test and clinical performance. The result of this study could tremendously accelerate the clinical application of “regulatory T cell therapy”, it is hoped that it could enter clinical test in the near future.
Research Implications
“This study discovers that a single dose of “antigen-specific CD8+ regulatory T cells” can effectively inhibit the allogeneic GVHD without affecting the general immune system of the humanized mice.”, says Dr Tu Wenwei, Associate Professor of Department of Paediatrics and Adolescent Medicine, HKU Li Ka Shing Faculty of Medicine, “Thus, this novel therapy will considerably reduce the dose immunosuppression drugs and the side effects. More importantly, as these CD8+ Tregs are recipient-specific, it might be no longer to consider HLA-matching, which will significantly increase the availability of bone marrows, if this Treg-based therapy can be successfully used in clinic finally.” The result will be further tested on human for clinical trial.
Research Background
Nowadays, BMT is extensively applied in treating malignant and non-malignant hematologic diseases, immunodeficiency, and some others blood system tumors. It can help extend the life expectancy of the patients, or even provide an eternal cure. Right now, there are over 100,000 patients undergoing BMT surgery worldwide every year. But, the GVHD induced by allogeneic transplantation dampened the treatment outcome.
Research Team
This research is led by Dr Tu Wenwei, Professor Lau Yu-lung of Department of Paediatrics and Adolescent, HKU Li Ka Shing Faculty of Medicine. Other investigators include Dr Zheng Jian, Dr Liu Yinping, and Liu Yuan. The research is supported by National Natural Science Foundation of China/Research Grants Council Joint Research Scheme, General Research Fund, Research Grants Council of Hong Kong, Area of Excellence program, and University Grants Committee of Hong Kong Special Administrative Region.
To use the press release photo(s) for any publishing, publicity and related purpose, photo courtesy should be given to “Li Ka Shing Faculty of Medicine, The University of Hong Kong”
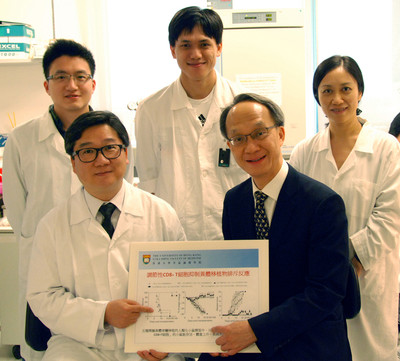
The research team led by Dr Tu Wenwei (left in the first row) and Professor Lau Yu-lung (right in the first row) of Department of Paediatrics and Adolescent Medicine discovers that “CD8+ regulatory T cells” can specify the antigen of bone marrow transplantation and it can effectively suppress the rejection effect against recipient. It might help solve the matching difficulty for bone marrow transplantation. Second row, start from the left are researchers Mr Liu Yuan, Dr Zheng Jian and Dr Liu Yinping.
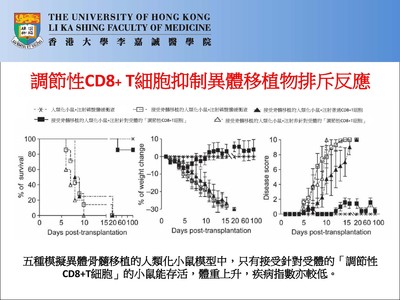
The graphs illustrate the allogeneic bone marrow transplantation on humanized mice model.