HKU Scientists Bring New Hopes to Translate Human Stem Cell Technologies to the Clinic
13 Jan 2011
Scientists at The University of Hong Kong Li Ka Shing Faculty of Medicine have taken stem cell research a few steps closer to the clinic in 2010. The team of cardiologists and scientists has successfully generated new human induced pluripotent stem cells (hiPSCs) that are free from animal products. These new hiPSCs were then used to derive different human cell types and tissues to study the potential clinical applications of stem cell therapy for treatment of critical limb ischemia – a major cause of limb amputation in elderly, as well as modeling of human genetic diseases which cause juvenile onset of ageing, such as progeria. The same technology and strategy can also be applied to more commonly encountered diseases like neurodegeneration and heart failure to provide insights into the disease development; and more importantly lead to clues for developing new therapeutic strategies, such as stem cell therapy.
Professor Tse Hung-fat, William M W Mong Professor in Cardiology of the Department of Medicine, The University of Hong Kong Li Ka Shing Faculty of Medicine says, “The patient-own hiPSCs provide an unlimited source of human live cells without the need to really operate on the patients to get tissue samples from different organs. This allows the scientists and clinicians to investigate the use of those cells for tissue regeneration, to study the disease process and to test the response of drugs in a culture dish. In the near future, this new technology should help clinicians to understand disease development and to provide insights for the development of novel treatment strategies, and thus bringing new hopes to translate human stem cell technologies to the clinic.”
New human induced pluripotent stem cells (hiPSCs) technology
Many patients with end-stage organ failure die while waiting for suitable organs for transplantation due to severe shortage of donor organs. As a result, scientists and clinicians worldwide have been looking into new strategies including stem cell therapy to repair damaged organs. In 2007, a group of Japanese scientists first successfully generated hiPSCs from human skin cells which behave like embryonic stem cells and can turn into all cell types of human bodies. Compared with embryonic stem cells, hiPSCs share the same genetic composition of the patients thereby eliminating potential immune rejection and ethical issue related to human embryonic stem cells. Hence, hiPSCs have been quickly emerged as one of the most promising cell sources for regenerative medicine. However, the current protocols to generate hiPSCs require the use of animal products, such as live mouse cells and animal serum, which make the cells unsuitable for any clinical use.
Breakthroughs in human stem cell researches by scientists in HKU
Recently, the HKU team has successfully eliminated the need of using any animal products in the generation of patient-own hiPSCs. The new hiPSCs can turn into all cell types in our bodies including heart cells, brain cells, vessel cells, and liver cells, like that of embryonic stem cells. This work has been published in the journal, Cellular Reprogramming. The HKU research team led by Dr David Siu Chung-wah, Clinical Assistant Professor of the Department of Medicine, The University of Hong Kong Li Ka Shing Faculty of Medicine, obtained patients’ skin cells, and reprogrammed them back to embryonic stem cell-like state using a newly designed protocol. The essence of the HKU protocol is the use of a special enzyme inhibitor to facilitate hiPSC generation in order to eliminate the need of live mouse cells and animal serum in the reprogramming process, which is a big step forward for future clinical application.
Another researcher in the team, Dr Lian Qizhou, Assistant Professor of the Department of Medicine and Eye Institute, The University of Hong Kong Li Ka Shing Faculty of Medicine, transplanted the mesenchymal stem cells (MSC), a subpopulation of more mature human stem cells, into the limbs of mice with poor blood supply due to damaged arteries. The MSCs can form new blood vessels and improve circulation of the limbs. Besides, the study has further demonstrated that MSC can further eliminate the risk of tumor formation after transplantation. This work provides the first proof-of-concept evidence to use hiPSC-based therapy to treat human cardiovascular diseases. Furthermore, this type of human stem cells derived from hiPSC is also more effective than the similar stem cells obtained from human bone marrow tissue. This type of cellular products derived from hiPSC also provides promises to treat different forms of cardiovascular diseases as they are patient-specific and eliminate the potential risk of immune rejection and ethical issue related to human embryonic stem cells. The work has been recently published in the top ranking cardiology journal, Circulation.
In addition to potential therapeutic application, hiPSC could be used as a tool to investigate human diseases. Professor Tse and Dr Lian in collaboration with researchers of the Stem Cell Consortium at A*STAR Institute of Medical Biology in Singapore have been using the new hiPSC technology to study the origins of progeria, a dreadful genetic disease that occurs one in every 8 million live births. The disease causes premature ageing in children, and most afflicted individuals die in their early teens due to the damages and degeneration in various organs of their bodies, resembling that of the elderly. Importantly, this rare disease may provide insights to the cause of human ageing. To understand the disease, researchers generate hiPSCs from the skin of a progeria patient and turn them into various types of cells like nerve cells, blood vessels cells, and MSCs. This allows the scientists and clinicians to model the disease in the laboratory and study the disease process occurred in different organs in a culture dish. The work has been recently published in top ranking stem cell research journal, Cell Stem Cell.
The Way forward
While the technological breakthroughs have moved the research closer to ultimate clinical uses, certain hurdles including the use of gene-transfer viruses have to be overcome. Active research in this area is ongoing in the HKU Department of Medicine. In fact, the HKU team is now building up a disease specific-hiPSC library in order to facilitate research in understanding, treating, and preventing human diseases.
About the research team
The HKU research team is formed by a group of clinicians and scientists at the Department of Medicine, the University of Hong Kong Li Ka Shing Faculty of Medicine. The team is led by Professor Tse Hung-fat, other key researchers include Dr David Siu Chung-wah, and Dr Lian Qizhou.
To use the press release photo(s) for any publishing, publicity and related purpose, photo courtesy should be given to “Li Ka Shing Faculty of Medicine, The University of Hong Kong”

Professor Tse Hung-fat, William M W Mong Professor in Cardiology of the Department of Medicine, The University of Hong Kong Li Ka Shing Faculty of Medicine, said the HKU protocol for generating human induced pluripotent stem cells helps to understand disease development and provide insights for the development of novel treatment strategies.
Dr David Siu Chung-Wah, Clinical Assistant Professor of the Department of Medicine, The University of Hong Kong Li Ka Shing Faculty of Medicine and his fellows successfully eliminated the need of using animal products in the generation of patient-own human induced pluripotent stem cells.

Dr Lian Qizhou, Assistant Professor of the Department of Medicine and Eye Institute, The University of Hong Kong Li Ka Shing Faculty of Medicine, and his team treated mice with poor blood supply due to damaged arteries, which is more effective than the similar stem cells obtained from human bone marrow tissue.
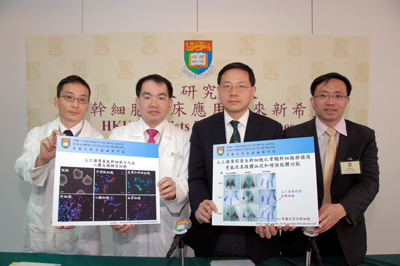
Members of The University of Hong Kong Li Ka Shing Faculty of Medicine who are in charge of the researches: (From left) Mr Kevin Lai Wing-hon, Senior Technical Officer, Department of Medicine; Dr David Siu Chung-Wah, Clinical Assistant Professor of the Department of Medicine; Professor Tse Hung-fat, William M W Mong Professor in Cardiology of the Department of Medicine and Dr Lian Qizhou, Assistant Professor of the Department of Medicine and Eye Institute.